Antibodies Offer a New Path for Fighting Flu
.jpg) By DONALD G. McNEIL Jr.
By DONALD G. McNEIL Jr.Published: February 22, 2009
In a discovery that could radically change how the world fights influenza, researchers have engineered antibodies that protect against many strains of the virus, including even the 1918 Spanish flu and the H5N1 bird flu.
The discovery, experts said, could lead to the development of a flu vaccine that would not have to be changed yearly. And the antibodies already developed can be injected as a treatment, going after the virus in ways that drugs like Tamiflu do not.
Clinical trials to prove that the antibodies are safe in humans could begin within three years, a researcher estimated.
“This is a really good study,” said Dr. Anthony S. Fauci, the director of the National Institute of Allergy and Infectious Diseases, who was not part of the study. “It’s not yet at the point of practicality, but the concept is really quite interesting.”
The work is so promising that Dr. Fauci’s institute will offer the researchers grants and access to its ferrets, which can catch human flu.
The study, done by researchers from Harvard Medical School, the Centers for Disease Control and Prevention and the Burnham Institute for Medical Research, was published Sunday in the journal Nature Structural & Molecular Biology.
In an accompanying editorial, Dr. Peter Palese, a leading flu researcher from Mount Sinai Medical School, said the researchers had apparently found “a viral Achilles’ heel.”
Dr. Anne Moscona, a flu specialist at Cornell University’s medical school, called it “a big advance in itself and one that shows what’s possible for other rapidly evolving pathogens.”
But Henry L. Niman, a biochemist who tracks flu mutations, was skeptical, arguing that human immune systems would have long ago eliminated flu were the virus as vulnerable in one spot as this discovery suggested. Also, he noted, protecting the mice in the study took huge doses of antibodies, which are expensive and cumbersome to infuse.
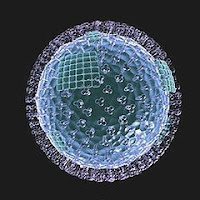
One team leader, Dr. Wayne A. Marasco of Harvard, said it began by screening a library of 27 billion antibodies he had created, looking for ones that take aim at the hemagglutinin “spikes” on the shells of flu viruses.
Antibodies are proteins normally produced by white blood cells that attach to invaders, either neutralizing them by clumping on or tagging them so that white cells can find and engulf them. They can be built in the laboratory and then “farmed” in plants, driving prices down, Dr. Marasco said.
The flu virus uses the lollipop-shaped hemagglutinin spike to invade nose and lung cells. There are 16 known types of spikes, H1 through H16.
The spike’s tip mutates constantly, which is why flu shots have to be reformulated each year. But the team found a way to expose the spike’s neck, which apparently does not mutate, and picked antibodies that clamped onto it. Once its neck is clamped, a spike can still penetrate a human cell, but it cannot unfold to inject the genetic instructions that take over the cell’s machinery to make more virus.
The team then turned the antibodies into full-length immunoglobulins and tested them in mice.
Immunoglobulin — antibodies derived from the blood of survivors of an infection — has a long history in medicine. As early as the 1890s, doctors injected blood from sheep that had survived diphtheria to save a girl dying of it. But there can be dangerous side effects, including severe immune reactions or accidental infection with other viruses.
The mice in the antibody experiments were injected before and after receiving doses of H5N1. In 80 percent of cases, they were protected. The team then showed that their new antibodies could protect against both H1 and H5 viruses. Most of the flu this season is H1, and experts still fear that the lethal H5N1 bird flu may start a human pandemic.
However, the other seasonal flu outbreaks each year are usually caused by H3 or B strains, so flu shots must also contain those. But there is always at least a partial mismatch because vaccine makers must pick from among strains circulating in February since it takes months to make supplies. By the time the flu returns in November, its “lollipop heads” have often mutated.
Therefore, other antibodies that clamp onto and disable H3 and B will have to be found before doctors even think of designing a once-a-lifetime flu shot. It is also unclear how long an antibody-producing vaccine will offer protection; new antibodies themselves fade out of the blood after about three weeks.
Dr. Marasco said that his team had already found a stable neck in the H3 and that they were “going after that one too.” They have not tried with B strains yet.
To make a vaccine work, researchers also need a way to teach the immune system to expose the spike’s neck for attack. It is hidden by the fat lollipop head, whose rapid mutations may act as a decoy, attracting the immune system.
As a treatment for people already infected with flu, Dr. Marasco said, the antibodies are “ready to go, no additional engineering needed.”
They will, of course, need the safety testing required by the Food and Drug Administration.
Antiflu drugs like Tamiflu, Relenza and rimantadine do not go after the hemagglutinin spike.
Tamiflu and Relenza inhibit neuraminidase (the “N” in flu names like H5N1), which has been described as a helicopter blade on the outside of the virus that chops up the receptors on the outside of the infected cell so the new virus being made inside can escape. Rimantidine is believed to attack a layer of the virus’s shell.














Post a Comment