A new drug test: SEWAGE
read more» Read more...
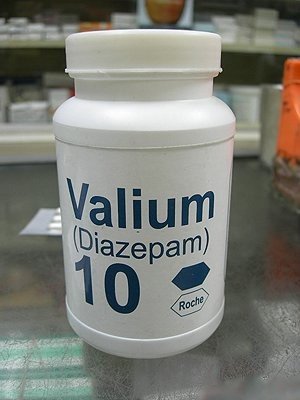 Diazepam , first marketed as Valium by Hoffmann-La Roche, is a benzodiazepine derivative drug.
Diazepam , first marketed as Valium by Hoffmann-La Roche, is a benzodiazepine derivative drug.
 Sildenafil citrate, sold under the names Viagra, Revatio and under various other names, is a drug used to treat male erectile dysfunction (impotence) and pulmonary arterial hypertension (PAH), developed by the pharmaceutical company Pfizer. Its primary competitors on the market are tadalafil (Cialis), and vardenafil (Levitra).
Sildenafil citrate, sold under the names Viagra, Revatio and under various other names, is a drug used to treat male erectile dysfunction (impotence) and pulmonary arterial hypertension (PAH), developed by the pharmaceutical company Pfizer. Its primary competitors on the market are tadalafil (Cialis), and vardenafil (Levitra).
 Warfarin (also known under the brand names of Coumadin, Jantoven, Marevan, and Waran) is an anticoagulant medication that is administered orally or, very rarely, by injection. It is also used as a pesticide against rats and mice.
Warfarin (also known under the brand names of Coumadin, Jantoven, Marevan, and Waran) is an anticoagulant medication that is administered orally or, very rarely, by injection. It is also used as a pesticide against rats and mice.
In its medical use, it is used for the prophylaxis of thrombosis and embolism in many disorders. Its activity has to be monitored by frequent blood testing for the international normalized ratio (INR). It is named for the Wisconsin Alumni Research Foundation.
Warfarin is a synthetic derivative of coumarin, a chemical found naturally in many plants, notably woodruff (Galium odoratum, Rubiaceae), and at lower levels in licorice, lavender, and various other species. Warfarin was originally developed as a rat poison; however, more modern poisons are much more potent and toxic (e.g., brodifacoum).
Warfarin and contemporary rodenticides belong to the same class of drugs (coumarins) and both decrease blood coagulation by interfering with vitamin K recycling. Warfarin inhibits vitamin K reductase, which is the enzyme responsible for recycling oxidated vitamin K back into the system. For this reason, drugs in this class are also referred to as vitamin K antagonists.
Mechanism of action
Warfarin inhibits the synthesis of biologically active forms of the vitamin K–dependent clotting factors II, VII, IX and X, as well as the regulatory factors protein C, protein S, and protein Z. Other proteins not involved in blood clotting, such as osteocalcin, or matrix Gla protein, may also be affected.
The precursors of these factors require carboxylation of their glutamic acid residues to allow the coagulation factors to bind to phospholipid surfaces inside blood vessels, on the vascular endothelium. The enzyme that carries out the carboxylation of glutamic acid is gamma-glutamyl carboxylase. The carboxylation reaction will proceed only if the carboxylase enzyme is able to convert a reduced form of vitamin K (vitamin K hydroquinone) to vitamin K epoxide at the same time. The vitamin K epoxide is in turn recycled back to vitamin K and vitamin K hydroquinone by another enzyme, the vitamin K epoxide reductase (VKOR).
Warfarin inhibits epoxide reductase (specifically the VKORC1 subunit), thereby diminishing available vitamin K and vitamin K hydroquinone in the tissues, which inhibits the carboxylation activity of the glutamyl carboxylase. When this occurs, the coagulation factors are no longer carboxylated at certain glutamic acid residues, and are incapable of binding to the endothelial surface of blood vessels, and are thus biologically inactive.
As the body stores of previously-produced active factors degrade (over several days) and are replaced by inactive factors, the anticoagulation effect becomes apparent. The coagulation factors are produced, but have decreased functionality due to undercarboxylation; they are collectively referred to as PIVKAs (proteins induced [by] vitamin K absence/antagonism), and individual coagulation factors as PIVKA-number (e.g. PIVKA-II). The end result of warfarin use, therefore, is to diminish blood clotting in the patient.
The initial effect of warfarin administration is to briefly promote clot formation. This is because the level of protein S is also dependent on vitamin K activity. Reduced levels of protein S lead to a reduction in activity of protein C (for which it is the co-factor) and therefore reduced degradation of factor Va and factor VIIIa. This then causes the hemostasis system to be temporarily biased towards thrombus formation, leading to a prothrombotic state.
This is one of the benefits of co-administering heparin, an anticoagulant that acts upon antithrombin and helps reduce the risk of thrombosis, which is common practice in settings where warfarin is loaded rapidly.
Uses
Medical use
Warfarin is prescribed to people with an increased tendency for thrombosis or as prophylaxis in those individuals that have already formed a blood clot (thrombus), which required treatment. This can help prevent formation of future blood clots and help reduce the risk of embolism (migration of a thrombus to a spot where it blocks blood supply to a vital organ). Common clinical indications for warfarin use are atrial fibrillation, artificial heart valves, deep venous thrombosis, pulmonary embolism, antiphospholipid syndrome and occasionally after myocardial infarction.
Dosing of warfarin is complicated by the fact that it is known to interact with many commonly-used medications and other chemicals that may be present in appreciable quantities in food. These interactions may enhance or reduce warfarin's anticoagulation effect. Many commonly-used antibiotics, such as metronidazole or the macrolides, will greatly increase the effect of warfarin by reducing the metabolism of warfarin in the body.
Other broad-spectrum antibiotics can reduce the amount of the normal bacterial flora in the bowel, which make significant quantities of Vitamin K, thus potentiating the effect of warfarin.
In addition, food that contains large quantities of Vitamin K will reduce the warfarin effect; and medical conditions such as hypo- or hyperthyroidism will alter the rate of breakdown of the clotting factors.
Therefore, in order to optimise the therapeutic effect without risking dangerous side-effects, such as bleeding, close monitoring of the degree of anticoagulation is required by blood testing (INR). During the initial stage, checking may be as often as every day; the intervals can be lengthened if the patient manages stable therapeutic INR levels on an unchanged warfarin dose.
When initiating warfarin therapy ("warfarinisation"), the doctor will decide how strong the anticoagulant therapy needs to be. The target INR level will vary from case to case dependent upon the clinical indicators, but tends to be 2-3 in most conditions. In particular, target INR will be 2.5-3.5 in patients with artificial (mechanical) heart valves.
The oral anticoagulant ximelagatran (Exanta) was expected to replace warfarin to a large degree when introduced; however, reports of hepatotoxicity (liver damage) prompted its manufacturer to withdraw it from further development. Other drugs offering the efficacy of warfarin without a need for monitoring, such as dabigatran, rivaroxaban, and idraparinux, are under development.
Pesticide use
Coumarins, a class of drugs of which warfarin is a member, are used as rodenticides for controlling rats and mice in residential, industrial, and agricultural areas. The active ingredient in rat poison is brodifacoum, which is sometimes referred to as a super-warfarin, because it is longer-acting than the drug warfarin. It is both odorless and tasteless.
It is effective when mixed with food bait, because the rodents will return to the bait and continue to feed over a period of days, until a lethal dose is accumulated (considered to be 1 mg/kg b.w./day over four to five days for warfarin; for brodifacoum, no reliable cumulative toxicity data are available at this time, but it could be concluded, given the similarity with other 4-hydroxycoumarin derivatives, that these would be in order of tens of µg/kg b.w./day for periods of 2-10 days). It may also be mixed with talc and used as a tracking powder, which accumulates on the animal's skin and fur, and is subsequently consumed during grooming.
The use as rat poison is now declining because many rat populations have developed resistance to warfarin.
The LD50 is 50–500 mg/kg. The IDLH value is 100mg/m³ (warfarin; various species). LD50(mouse, oral) = 0.40 mg/kg; (rat, oral) = 0.27 mg/kg (brodifacoum). The IDLH value for brodifacoum is not defined, but given the toxicity of brodifacoum, it would be substantially lower, perhaps less than 1/100 of the warfarin value, i.e., <1 id="Side-effects" name="Side-effects">
Side-effects
Hemorrhage
The only common side-effect of warfarin is hemorrhage (bleeding). The risk of severe bleeding is small but definite (1-2% annually) and any benefit needs to outweigh this risk when warfarin is considered as a therapeutic measure.
Risk of bleeding is augmented if the INR is out of range (due to accidental or deliberate overdose or due to interactions), and may cause hemoptysis (coughing up blood), excessive bruising, bleeding from nose or gums, or blood in urine or stool.
The risks of bleeding is increased when warfarin is combined with antiplatelet drugs such as clopidogrel, aspirin, or nonsteroidal anti-inflammatory drugs. The risk may also be also increased elderly patients and in patients on hemodialysis.
Warfarin necrosis
A feared (but rare) complication of warfarin is warfarin necrosis, which occurs more frequently shortly after commencing treatment in patients with a deficiency of protein C. Protein C is an innate anticoagulant that, like the procoagulant factors that warfarin inhibits, requires vitamin K-dependent carboxylation for its activity.
Since warfarin initially decreases protein C levels faster than the coagulation factors, it can paradoxically increase the blood's tendency to coagulate when treatment is first begun (many patients when starting on warfarin are given heparin in parallel to combat this), leading to massive thrombosis with skin necrosis and gangrene of limbs. Its natural counterpart, purpura fulminans, occurs in children who are homozygous for protein C mutations.
Osteoporosis
After initial reports that warfarin could reduce bone mineral density, several studies have demonstrated a link between warfarin use and osteoporosis-related fracture. A 1999 study in 572 women taking wafarin for DVT, risk of vertebral fracture and rib fracture was increased; other fracture types did not occur more commonly.
A 2002 study looking at a randomly selected selection of 1523 patients with osteoporotic fracture found no increased exposure to anticoagulants compared to controls, and neither did stratification of the duration of anticoagulation reveal a trend towards fracture.
A 2006 retrospective study of 14,564 Medicare recipients showed that warfarin use for more than one year was linked with a 60% increased risk of osteoporosis-related fracture in men; there was no association in women.
The mechanism was thought to be either reduced intake of vitamin K, which is necessary for bone health, or interaction by warfarin with carboxylation of certain bone proteins.
Purple toe syndrome
Another rare complication that may occur early during warfarin treatment (usually within 3 to 8 weeks) is purple toe syndrome. This condition is thought to result from small deposits of cholesterol breaking loose and flowing into the blood vessels in the skin of the feet, which causes a blueish purple color and may be painful. It is typically thought to affect the big toe, but it affects other parts of the feet as well, including the bottom of the foot (plantar surface). The occurrence of purple toe syndrome may require discontinuation of warfarin.
Pharmacology
3mg (blue), 5mg (pink) and 1mg (brown) warfarin tablets (UK colours)
Pharmacokinetics
Warfarin consists of a racemic mixture of two active optical isomers - R and S forms - each of which is cleared by different pathways. S-warfarin has five times the potency of the R-isomer with respect to vitamin K antagonism.
Warfarin is slower-acting than the common anticoagulant heparin, though it has a number of advantages. Heparin must be given by injection, whereas warfarin is available orally. Warfarin has a long half-life and need only be given once a day. Heparin can also cause a prothrombotic condition, heparin-induced thrombocytopenia (an antibody-mediated decrease in platelet levels), which increases the risk for thrombosis.
Warfarin's long half life, on the other hand, means it often takes several days to reach therapeutic effect. Furthermore, if given initially without additional anticoagulant cover, it can increase thrombosis risk. For these main reasons, hospitalised patients are usually given heparin first, and are then moved on to warfarin.
Antagonism
Warfarin can be reversed with vitamin K, or for rapid reversal (e.g., in case of severe bleeding), with fresh frozen plasma, but this treatment is being replaced by use of prothrombin complex concentrate.
Details on reversing warfarin are provided in clinical practice guidelines from the American College of Chest Physicians. For patients with an international normalized ratio (INR) between 4.5 and 10.0, 1 mg of oral vitamin K is effective.
Pharmacogenomics
Warfarin activity is determined partially by genetic factors. The American Food and Drug Administration "highlights the opportunity for healthcare providers to use genetic tests to improve their initial estimate of what is a reasonable warfarin dose for individual patients" .
VKORC1
Polymorphisms in the vitamin K epoxide reductase complex 1 (VKORC1) gene explain 30% of the dose variation between patients: particular mutations make VKORC1 less susceptible to suppression by warfarin There are a main haplotypes that explain 25% of variation: low-dose haplotype group (A) and a high-dose haplotype group (B). For the three combinations of the haplotypes, the mean daily maintenance dose of warfarin was:
A/A: 2.7+/-0.2 mg
A/B: 4.9+/-0.2 mg
B/B: 6.2+/-0.3 mg
VKORC1 polymorphisms also explain why African Americans are relatively resistant to warfarin (higher proportion of group B haplotypes), while Asian Americans are more sensitive (higher proportion of group A haplotypes).
CYP2C9
CYP2C9 is an isozyme of cytochrome P450. Polymorphisms of CYP2C9 explain another 10% of variation in warfarin dosing, mainly among Caucasian patients as these variants are rare in African American and most Asian populations. A meta-analysis of mainly Caucasian patients found :
CYP2C9*2 allele:
present in 12.2% of patients
mean reduction was in warfarin dose was 0.85 mg (17% reduction)
relative bleeding risk was 1.91
CYP2C9*3 allele:
present in 7.9% of patients
mean reduction was in warfarin dose was 1.92 mg (37% reduction)
relative bleeding risk was 1.77
Loading regimens
Because of warfarin's poorly-predictable pharmacokinetics, several researchers have proposed algorithms for commencing warfarin treatment:
The Kovacs 10 mg algorithm was better than a 5 mg algorithm.
The Fennerty 10 mg regimen is for urgent anticoagulation
The Tait 5 mg regimen is for "routine" (low-risk) anticoagulation (summary)
From a cohort of orthopedic patients, Millican et al derived an 8-value model, including CYP29C and VKORC1 genotype results, that could predict 80% of the variation in warfarin doses. It is awaiting validation in larger populations and has not been reproduced in those who require warfarin for other indications.
Adjusting the maintenance dose
Recommendations by the American College of Chest Physicians have been distilled to help manage dose adjustments.
Guidelines for self testing and home monitoring
Patients are making increasing use of self-testing and home monitoring of oral anticoagulation. International guidelines were published in 2005 to govern home testing, by the International Self-Monitoring Association for Oral Anticoagulation.
The international guidelines study stated, "The consensus agrees that patient self-testing and patient self-management are effective methods of monitoring oral anticoagulation therapy, providing outcomes at least as good as, and possibly better than, those achieved with an anticoagulation clinic. All patients must be appropriately selected and trained. Currently-available self-testing/self-management devices give INR results that are comparable with those obtained in laboratory testing."
Interactions and contraindications
There are many drug-drug interactions with warfarin, and its metabolism varies greatly between patients. Some foodstuffs have also been reported to interact with warfarin. This makes finding the correct dosage difficult, and accentuates the need of monitoring; when initiating a medication that is known to interact with warfarin (e.g. simvastatin), INR checks are increased or dosages adjusted until a new ideal dosage is found.
Warfarin cannot be given to pregnant women, especially in the first trimester, as it is a teratogen causing deformations of the face and bones. During the third trimester, antepartum hemorrhage can occur. Instead of warfarin, low molecular weight heparin is generally used. (See anticoagulation in pregnancy.)
Excessive use of alcohol is also known to affect the metabolism of warfarin and can elevate the INR. Patients are often cautioned against the excessive use of alcohol while taking warfarin. A common recommendation is limiting the maximum daily intake to no more than a few drinks. Patients suffering from liver damage or alcoholism are usually treated with heparin injections instead.
Warfarin also interacts with the many herbs, including - but not limited to - the following:
Ginkgo (a.k.a. Ginkgo Biloba), which is commonly used to increase brain blood flow, prevent dementia, and improve memory. However, ginkgo may increase blood pressure, and may increase bleeding, especially in people already taking certain anti-clotting medications such as warfarin.
St. John's Wort is commonly used to help with mild to moderate depression. However, it may prolong the effects of certain anesthetic drugs and reduce the effects oral contraceptives and anti-organ transplant rejection medications, and interfere with warfarin.
Ginseng is commonly used to help with fatigue and weakness. However, ginseng may increase blood pressure and heart rate and may increase bleeding, especially in people already taking certain anti-clotting medications such as warfarin.
Garlic (as a supplement, not in the diet) is commonly used to help lower high cholesterol levels, high triglycerides, and high blood pressure. However, may increase bleeding especially in people already taking certain anti-clotting medications such as warfarin.
Ginger is commonly used to help nausea and poor digestion. However, it may increase bleeding, especially in patients already taking certain anti-clotting medications such as warfarin.
History
The early 1920s saw the outbreak of a previously unrecognized disease of cattle in the northern United States and Canada. Cattle would die of uncontrollable bleeding from very minor injuries, or sometimes drop dead of internal hemorrhage with no external signs of injury. In 1921, Frank Schofield, a Canadian veterinarian, determined that the cattle were ingesting moldy silage made from sweet clover that functioned as a potent anticoagulant. In 1929, North Dakota veterinarian Dr L.M. Roderick demonstrated that the condition was due to a lack of functioning prothrombin.
The identity of the anticoagulant substance in moldy sweet clover remained a mystery until 1940 when Karl Paul Link and his student Harold Campbell, chemists working at the University of Wisconsin, determined that it was the coumarin derivative 4-hydroxycoumarin.
Over the next few years, numerous similar chemicals were found to have the same anticoagulant properties. The first of these to be widely commercialized was dicoumarol, patented in 1941. Link continued working on developing more potent coumarin-based anticoagulants for use as rodent poisons, resulting in warfarin in 1948. (The name warfarin stems from the acronym WARF, for Wisconsin Alumni Research Foundation + the ending -arin indicating its link with coumarin.) Warfarin was first registered for use as a rodenticide in the US in 1948, and was immediately popular; although it was developed by Link, the WARF financially supported the research and was granted the patent.
After an incident in 1951, where a naval enlisted man unsuccessfully attempted suicide with warfarin and recovered fully, studies began in the use of warfarin as a therapeutic anticoagulant. It was found to be generally superior to dicoumarol, and in 1954 was approved for medical use in humans. A famous early patient prescribed warfarin was Dwight Eisenhower, president of the USA, subsequent to his heart attack in 1955.
The exact mechanism of action remained unknown until it was demonstrated, in 1978, that warfarin inhibited epoxide reductase and hence interfered with vitamin K metabolism.
A 2003 theory posits that warfarin was used by a conspiracy of Lavrenty Beria, Nikita Khrushchev and others to poison Soviet leader Joseph Stalin. Warfarin is tasteless and colorless, and produces symptoms similar to those that Stalin exhibited.
Other coumarins
In some countries, other coumarins are used instead of warfarin, such as acenocoumarol and phenprocoumon. These have a shorter (acenocoumarol) or longer (phenprocoumon) half-life, and are not completely interchangeable with warfarin.
Source : http://www.wikipedia.org/wiki/Warfarn
©Template by Dicas Blogger.