Findings May Lead to First Approved Treatment for Myelofibrosis
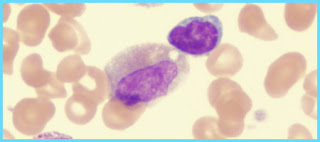
Myelofibrosis is a rare but serious disorder in which the bone marrow is replaced by scar tissue. There is no currently approved treatment for the disease, but a phase I/II clinical study of an experimental drug produced by Incyte Corp. of Delaware may possibly lead to the first medical option to reduce spleen size.
One of the primary symptoms of myelofibrosis is an enlarged spleen. Because the scarring of the bone marrow causes anemia, both the liver and the spleen attempt to make blood cells, which causes the organs to swell.
The new pill, called INCB18424 was found in a small study of 153 patients to reduce the size of the spleen of over half of the patients by 50% in an average of two weeks to one month, avoiding surgery to remove the organ called a splenectomy.
Also, fewer patients than expected progressed to a more severe form of the disorder called acute myeloid leukemia, a cancer that starts in the bone marrow and affects the normal production of white blood cells.
“This is a disease for which patients don’t have a therapy,” said Srdan Verstovsek, lead author and an associate professor in the Department of Leukemia at the University of Texas MD Anderson Cancer Center in Houston. The results, particularly the reduction of spleen size, have been “unbelievable,” he said.
The pill was also found to lessen other common symptoms, such as weight loss, fatigue and night sweats. Unfortunately, however, the medicine did not effectively address anemia, which in myelofibrosis patients often requires blood transfusions and medications called recombinant erythropoietin to help stimulate red blood cell production.
Incyte plants to initiate the third and final stage of human trials required for US approval of INCB18424.
If approved, the drug will likely be marketed by Novartis outside the US, according to Reuters.
read more» Read more...