New Cancer Drug To Be Tested In Wichita
 Increasing access to Phase I clinical trials throughout the state is becoming a reality today as officials from The University of Kansas Cancer Center and the Cancer Center of Kansas announced opening Nanotax, a Phase I clinical trial in Wichita.
Increasing access to Phase I clinical trials throughout the state is becoming a reality today as officials from The University of Kansas Cancer Center and the Cancer Center of Kansas announced opening Nanotax, a Phase I clinical trial in Wichita.This is the first Phase I clinical trial discovered, developed and delivered by The University of Kansas Cancer Center, which is a critical component of achieving National Cancer Institute (NCI) designation.
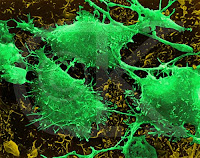
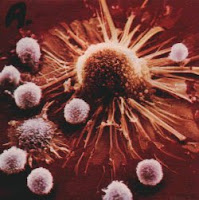
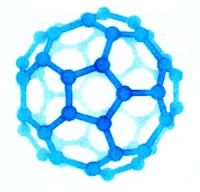
Often the side effects of chemotherapy are as difficult for patients to cope with as the cancer itself. Nanotax, a reformulation of the commonly used chemotherapy drug Paclitaxel, enables the drug to be mixed with water, which significantly reduces its negative side effects.
Nanotax initially opened at The University of Kansas Cancer Center in June 2008. The trial will enroll approximately 21 patients total with advanced peritoneal cancers.
“Our mission is to ensure everyone across the state has access to cutting-edge clinical trials no matter where they live,” said Roy A. Jensen, MD, director of The University of Kansas Cancer Center. “Opening the Phase I clinical trial Nanotax in Wichita moves us closer to fulfilling this mission by giving patients more options close to home.”
Eligible patients can participate in the trial at the Cancer Center of Kansas, under the direction of Shaker Dakhil, MD, FACP, and Thomas Schulz, MD. Drs. Dakhil and Schulz are nationally known oncologists who currently conduct 116 Phase II and Phase III clinical trials.
“The Cancer Center of Kansas has provided patients access to cutting-edge clinical trials for many years,” said Shaker Dakhil, MD, president of the Cancer Center of Kansas. “This Phase I clinical trial will complement the already extraordinary program we have in place and will allow us to offer more options to our patients.”
The trial also complements the Community Clinical Oncology Program (CCOP) grant the Cancer Center of Kansas holds from the National Cancer Institute (NCI), which provides access to Phase II and Phase III clinical trials.
Funding to support the infrastructure needed to conduct a Phase I clinical trial was provided by the Kansas Bioscience Authority (KBA) earlier this year through the Collaborative Cancer Research Initiative program.
The technology that led to the discovery of Nanotax was developed by University of Kansas researchers and was licensed to CritiTech, Inc., a Lawrence-based biotechnology firm, which patented, developed, produced and filed the investigational new drug application with the Food and Drug Administration (FDA). Collaborating with CritiTech and Beckloff and Associates, researchers at The University of Kansas Cancer Center developed the clinical trial.
Demonstrating the ability to translate discoveries made in the lab into new drugs and enrolling patients onto the clinical trial of the new drug helps The University of Kansas Cancer Center meet key criteria needed to apply for NCI designation. Showing the Cancer Center’s ability to conduct translational research while extending the benefits of its research beyond its center is a hallmark of an NCI-designated center.
Source : www.kake.com
read more» Read more...