The Daily Mail says that British scientists have created a “new drug that 'kills' leukaemia - even in worst affected adults”. The research behind this news found that the drug, called PBOX-15, could kill cancerous cells extracted from people with chronic lymphocytic leukaemia (CLL). The drug also killed cells that were resistant to an approved anti-cancer drug.
Several newspapers have discussed this laboratory study, highlighting the fact that this was early research and that any potential treatment using this chemical is a long way off. A quick glance at the Daily Mail’s headline may suggest that this drug has been tested in patients, but this was not the case. Instead, the study was carried out on cells grown in the laboratory and cannot be used to predict what other effects PBOX-15 might have in a living body.
Much more research will be needed to identify how safe and effective this drug is in animals before it can be potentially tested in humans. Drugs that show promise in the lab may prove unsafe or ineffective in later animal testing, which means they will not get developed into to useable medications.
Where did the story come from?
The research was carried out by Dr Anthony M McElligott and colleagues at Trinity College
Dublin and other centres in Ireland, Northern Ireland and Italy. It was published in the peer-reviewed journal Cancer Research. The research was funded by Enterprise Ireland, Cancer Research Ireland and the Higher Education Authority of Ireland.
The newspapers correctly reported that the development of this drug is at an early stage and that it may be years before it can be used. However, the Daily Mail’s headline that the drug “‘kills’ leukaemia - even in worst affected adults” may lead people to believe that this drug has been tested in patients, which is not the case. Headlines in other news sources, such as BBC News and The Daily Telegraph, are more accurate and simply stating that the drug has been shown to kill leukaemia cells.
What kind of research was this?
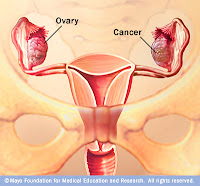
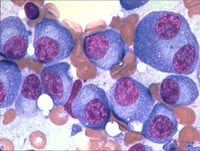
This laboratory study looked at the effects of a chemical called PBOX-15 (pyrrolo-1,5-benzoxazepine-15) on leukaemia cells extracted from people with chronic lymphocytic leukaemia (CLL). The authors say that new treatments are needed for CLL, particularly for patients who do not respond well to existing therapies.
There are many stages involved in developing and testing potential new drugs. The earlier stages usually involve laboratory studies, such as this one, which are used to identify the effects of the drug on affected cells and tissues. This early research is important for directing further study but cannot reliably predict what other effects a drug such as PBOX-15 might have in a living body. This study will need to be followed up with further research to assess how safe and effective the drug is in animals.
What did the research involve?
The researchers took blood samples from 55 CLL patients who had not yet begun treatment for CLL. From these samples, they isolated white blood cells that were affected by CLL and exposed them to PBOX-15 in the laboratory to see whether the cells died. The researchers also compared the effects of PBOX-15 with the effects of fludarabine on CLL cells, a chemotherapy drug used to treat CLL. They also carried out experiments to look at the effect of PBOX-15 on normal bone marrow cells taken from three healthy donors.
What were the basic results?
The researchers found that PBOX-15 could kill CLL cells in the laboratory. The drug could also kill CLL cells whose characteristics would normally be expected to cause a poor outcome of the disease. Comparison testing showed that PBOX-15 was more effective than fludarabine at killing fludarabine-sensitive CLL cells. PBOX-15 also killed CLL cells that had a genetic mutation that made them resistant to fludarabine treatment. Testing on three donor bone marrow samples found that PBOX-15 was more toxic to CLL cells than to normal bone marrow cells.
How did the researchers interpret the results?
The researchers concluded that PBOX-15 can kill both high-risk and low-risk CLL cells, and shows “significant clinical potential”.
Conclusion
Although the study shows that PBOX-15 can kill isolated human CLL cells in the laboratory, it cannot reliably predict what other effects it might have in a living body.
There are many stages to developing and testing potential new drugs, which can take many years and are not guaranteed to be successful. The early development stages involve laboratory studies such as this one, which are used identify the effects of the drug on affected cells and tissues. These early tests are important to establish whether future research is worthwhile.
Following the results of this initial study, the drug seems to be a candidate for further research, which would need to identify how safe and effective this drug is in animals before it could be tested in humans.
read more»
Read more...
 A radical new drug used to treat patients suffering painful sensitivity to sunlight could prevent skin cancer or be copied by the tanning industry.
A radical new drug used to treat patients suffering painful sensitivity to sunlight could prevent skin cancer or be copied by the tanning industry.