DR. MARK STILLMAN, the director of the Center for Headache and Pain at the Cleveland Clinic, has a treatment for people with frequent migraines: he injects Botox around the head and neck.
DR. MARK STILLMAN, the director of the Center for Headache and Pain at the Cleveland Clinic, has a treatment for people with frequent migraines: he injects Botox around the head and neck.
Dr. Andrew Blitzer, the director of the Center for Voice and Swallowing Disorders at St. Luke’s-Roosevelt Hospital Center in Manhattan, has an antidote for speech impediments caused by vocal cord problems: he injects Botox into the larynx.
Dr. Fredric Brandt, a dermatologist in Manhattan and Coral Gables, Fla., has a novel procedure for oily skin and skin redness.
You guessed it: Botox.
Over the last decade, Botox has become a synonym for the eradication of wrinkles, a kind of shorthand for the entire enterprise of cosmetic medicine. But now, with the popularization of new medical uses, therapeutic applications of the drug are poised to outstrip the cosmetic treatment in both revenue and prominence.
In the hunt to discover the next blockbuster medical use for Botox, doctors have injected it experimentally into muscles and glands all over the body, making it medicine’s answer to duct tape. According to recent medical journals, physicians have used it to treat chewing problems, swallowing problems, pelvic muscle spasms, drooling, hair loss, anal fissures and pain from missing limbs.
“We see it as a molecule that keeps on giving. As we understand it more, it gives us new ideas of how to use it,” says Dr. Mitchell F. Brin, a neurologist who is the chief scientific officer for Botox at Allergan, the drug’s maker.
No other therapeutic agent “has so many demonstrated uses,” he says.
But some health advocates worry that doctors are widely adopting novel uses for Botox before federal guidance and rigorous clinical studies have established safe and effective dosages for the new treatments.
“It’s trial and error with a nerve poison,” says Dr. Sidney M. Wolfe, the director of the health research group at Public Citizen, a consumer advocacy group. Last year, the group petitioned the Food and Drug Administration to require a warning label for injectable toxins.
BOTOX is a purified form of botulinum toxin, a nerve poison produced by the bacteria that cause botulism, a disease that paralyzes muscles and can be fatal. Injections of Botox act like minuscule poison darts that temporarily blunt chemical nerve signals to certain muscles or glands, reducing their activity.
The F.D.A. has approved Botox to treat four problems: eye muscle disorders, neck muscle disorders, excessive sweating — and that deadly age giveaway, eyebrow furrows. But Allergan, a $14.5 billion specialty pharmaceutical company, owns or has applied for patents on more than 90 uses for the drug.
Dr. Brin of Allergan says Botox has a long safety track record — backed by 30 years of favorable research, studies on 11,000 people worldwide and 17 million treatments in the United States since 1994.
“That safety profile has enabled us to continue to explore the product in deeper parts of the body and in more novel areas,” Dr. Brin says. Allergan does not promote unapproved uses of the drug, he says.
Botox was developed in the 1970s by Dr. Alan Scott, an ophthalmologist in San Francisco who was searching for a cure for crossed eyes. He theorized that minute doses of a nerve poison used to weaken the muscles that pull crossed eyes inward could treat the malady, and he experimented with a variety of paralytic agents.
Then a biochemist who had isolated and purified a strain of botulinum toxin for potential military use as a biological weapon sent Dr. Scott a sample. It worked.
Dr. Scott named the new drug Oculinum. In 1989, the F.D.A. approved it to treat crossed eyes and twitching eyelids. Allergan bought Oculinum in 1991 for about $9 million, rebranding it Botox. When David E. I. Pyott became chief executive of the company in 1998, Botox had $90 million in annual sales. Last year, sales topped $1 billion.
“Nobody at Allergan understood how big a gold mine they were sitting on,” Mr. Pyott says.
Drug companies often rely on multiple products to fill their pipelines. But at Allergan, Botox became a virtual pipeline in and of itself after the arrival of Mr. Pyott, who recognized that it was a medication that could be serially reincarnated for other applications.
Doctors, who are permitted to use approved drugs in unapproved ways as they deem appropriate, were already using Botox off-label at the time on body parts other than eye muscles. Some physicians reported that patients had unexpected side effects — fewer headaches, for example, or smoother skin — after they had Botox.
Mr. Pyott invested heavily in expanding in-house research and encouraged doctors to formalize their anecdotal observations with published research. He also recognized that some Americans would be willing to pay handsomely for injections that tempered wrinkles. To prove the efficacy of the drug, the company sponsored clinical trials to use Botox for cosmetic medical purposes and for other muscle disorders.
Over the last nine years, the F.D.A. has approved Botox to treat neck muscle spasms and to hinder excessive sweating. The agency also approved the same drug, under the name Botox Cosmetic, to smooth forehead wrinkles.
Last year, Botox had worldwide sales of $1.3 billion, divided about equally between cosmetic and medical uses. Among botulinum toxins, Botox has an 83 percent share of the market, Allergan said.
But, with competing toxins set to enter the American market, Allergan has positioned Botox for other medical uses. Mr. Pyott says he expects therapeutic sales of the drug to soon eclipse sales of Botox Cosmetic.
Health insurers sometimes cover medical uses of Botox; a treatment for a clenched jaw might cost $1,000 every three months, for example. But for cosmetic treatments, which dipped slightly at the end of last year, consumers must pay cash.
“The therapeutic will end up being bigger than the cosmetic even if the economy recovers because there are some big unmet medical needs there,” Mr. Pyott says.
In the next few months, the company is expecting federal approval to market the drug for stroke victims suffering from limb tightness or spasms.
Later this year, Allergan plans to seek approval to market the drug for chronic migraine headaches, Mr. Pyott said. He also said the company eventually plans to seek F.D.A. approval to market Botox for benign enlarged prostate.
But many doctors are not waiting for federal sanction to inject Botox for these and other disorders. While Allergan doesn’t break down Botox sales, Gary Nachman, an analyst at Leerink Swann, an investment bank, estimates that perhaps as much as half of Botox sales already come from off-label uses.
“It’s the magic bullet,” says Mr. Nachman.
BOTOX is so widely adopted in medicine — and ingrained in popular culture — that some doctors don’t think that novel uses are experiments.
Several years ago, Dr. Kamran Jafri, a facial surgeon in Manhattan, started injecting Botox just under the skin of the face, a technique that he says reduces pore size, blotchiness and oily skin.
“Dosing is by trial and error,” Dr. Jafri says. “I don’t think it’s experimental because it’s a treatment I’ve been doing a lot and it’s been working.”
Such ad hoc uses of Botox are perfectly legal for doctors. But some medical professionals are concerned that doctors are experimenting with and adopting Botox therapy before clinical trials and government approval have established safe doses for new indications — and without definitive proof that the new treatments work.
While life-threatening complications following use of Botox and other botulinum toxins are rare, a few people have died after they were treated. In some cases, the toxin has spread from the injection site, causing serious swallowing and breathing problems. For example, several children with cerebral palsy died after receiving large doses in their limbs.
“It is possible to over-inject. This is a poison,” says Dr. Frederick Burgess, the chief of anesthesia at the V.A. Medical Center in Providence, R.I. “Things can go wrong. It is rare, but it happens.”
Last year, Public Citizen petitioned the F.D.A., asking for a stronger warning on botulinum toxins that would emphasize the risk of diffusion from the injection site and the need for patients to seek immediate medical care for swallowing or breathing difficulties. The Canadian health authority instituted such a labeling change earlier this year.
Mr. Pyott of Allergan says that there have been a few serious problems following Botox injections — but not necessarily directly caused by the drug. Some patients had serious illnesses prior to treatment, he said.
“Physicians have experimented with higher and higher doses,” Mr. Pyott says. “Like any drug, if you take too much, you can have side effects.”
The F.D.A is reviewing the safety of botulinum toxins, according to an agency press release. Last year, the agency also postponed approval of a new toxin called Dysport for use in neck muscle problems. The F.D.A. asked the manufacturer to first develop a plan for communicating the risk of the drug to doctors and patients.
On Monday, the F.D.A. is due to issue a decision on the cosmetic version of Dysport, called Reloxin.
Johnson & Johnson is also developing an anti-wrinkle injection called PureTox.
But industry analysts predicted that the F.D.A. would postpone approving any new botulinum toxins until regulators have finalized a stronger warning label for all of the brands.
WHEN Mr. Pyott arrived at Allergan, it specialized in eye-care pharmaceuticals. Over the last decade, he has turned it into the house that Botox built, expanding credibility for the drug in various medical specialties by buying complementary businesses.
To solidify Allergan’s dominance in appearance medicine, for example, the company spent $3.2 billion in 2006 to acquire Inamed, a leading maker of skin-plumping injections and breast implants. In preparation for the planned introduction of Botox as a treatment for headaches, overactive bladder and enlarged prostates, the company has also established itself in neurology and urology by developing or marketing other specialty drugs, Mr. Pyott says.
The possibility of lucrative new uses for Botox has not gone unnoticed. After rumors of a possible merger with GlaxoSmithKline last month, Allergan stock rose almost 24 percent over the course of two days, to $48.95; it now trades at $47.47. Both companies declined to comment on merger rumors.
“This is a bad time to sell because they are not going to get rewarded for all of the wonderful stuff in the pipeline,” says Ronny Gal, an analyst at Sanford C. Bernstein. “I would stay independent for a couple of years.”
Mr. Gal says sales of Botox could double within the next five to seven years, provided that the F.D.A. approves new major medical uses. One million people or more might seek Botox injections for chronic headaches, while the audience for benign enlarged prostate would be “practically every man over the age of 75,” Mr. Gal says.
MR. PYOTT has a master plan, meanwhile, to expand the Botox franchise even further. The company is developing new iterations of the drug intended to treat specific targets, such as pain receptors, without weakening muscles.
Allergan also owns or has applied for patents on dozens of other uses for its toxin, a move to pre-empt competitors from marketing their products for expanded uses.
“I feel a little bit like I am sitting with a beautiful vessel inside the harbor but I forgot to give you the map to where our mines are,” Mr. Pyott says of the Botox patents that he said were filed in different countries. “There could be a big bang when you hit one of our patents.”
But Mr. Gal, the analyst, devoted his Christmas vacation to unearthing about 90 patent applications worldwide by Allergan. These included Botox for sinus headache, fibromyalgia pain, ulcers, inner ear disorders and uterine problems as well as appearance treatments like “buttock deformity.”
Nevertheless, there are still a few ailments that Botox does not claim to solve. Botox doesn’t work on stuttering, for example, because it involves too many parts of the anatomy — including the lips, the larynx and the tongue, says Dr. Brin of Allergan.
“Stuttering is too complicated,” Dr. Brin says a little wistfully. “It didn’t pan out.”
Source : www.nytimes.com
read more»
Read more...
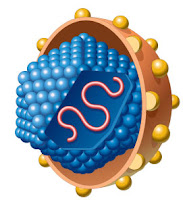
 A new drug which targets a genetic mutation found in 50 percent to 60 percent of melanoma cases, 10 percent to 15 percent of colorectal tumors and 8 percent of other solid tumors, caused tumor shrinkage and extended progression-free survival among patients during a Phase 1 clinical trial. Igor Puzanov, M.D., assistant professor of Medicine, and Jeffrey A. Sosman, M.D., professor of Medicine and Ingram Professor of Cancer Research, led Vanderbilt-Ingram Cancer Center’s participation in the multi-center study. Puzanov delivered the initial findings from the study during a poster session May 31 at the American Society of Clinical Oncology conference in Orlando, Fla.
A new drug which targets a genetic mutation found in 50 percent to 60 percent of melanoma cases, 10 percent to 15 percent of colorectal tumors and 8 percent of other solid tumors, caused tumor shrinkage and extended progression-free survival among patients during a Phase 1 clinical trial. Igor Puzanov, M.D., assistant professor of Medicine, and Jeffrey A. Sosman, M.D., professor of Medicine and Ingram Professor of Cancer Research, led Vanderbilt-Ingram Cancer Center’s participation in the multi-center study. Puzanov delivered the initial findings from the study during a poster session May 31 at the American Society of Clinical Oncology conference in Orlando, Fla.