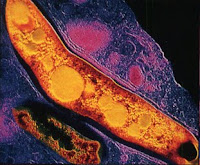
New Drug Boosts HCV Clearance
 Most hepatitis C patients who are initially unresponsive to standard therapy were able to achieve sustained virologic responses when the investigational drug boceprevir was added, a researcher reported here.
Most hepatitis C patients who are initially unresponsive to standard therapy were able to achieve sustained virologic responses when the investigational drug boceprevir was added, a researcher reported here.Sustained responses were seen in 55% of patients receiving 44 weeks of boceprevir after showing no virologic response to four weeks of pegylated interferon-alfa-2b (PEGIntron) and ribavirin (Rebetol) in a Phase II trial, said Paul Kwo, MD, of Indiana University in Indianapolis.
Kwo, speaking here at the American Association for the Study of Liver Disease meeting, was reporting on two secondary analyses of data from the SPRINT-1 trial of boceprevir, an inhibitor of the hepatitis C virus (HCV) NS3 protease enzyme.
He had presented the main findings of the 520-patient study earlier this year at the European Association for the Study of the Liver meeting in Copenhagen.
Boceprevir is one of two HCV protease inhibitors in late-stage development, the other being telaprevir. (See DDW: Telaprevir Improves HCV Clearance in Resistant Patients) Phase III trials of both drugs are now under way.
In the SPRINT-1 trial, treatment-naive patients were randomized to five treatment arms, including one in which patients only received pegylated interferon and ribavirin, two involving immediate treatment with all three agents, and two in which boceprevir started after an initial, four-week lead-in with interferon and ribavirin.
All patients had HCV genotype 1a or 1b, mostly the former.
The secondary analyses reported here focused only this last treatment strategy, with patients receiving either 24 or 44 weeks of triple therapy following the four-week, two-drug lead-in.
Boceprevir was dosed at 800 mg three times a day.
In patients with no response to the lead-in -- defined as a reduction in HCV RNA loads of less than ten-fold -- 25% of those receiving boceprevir for 24 weeks still showed viral clearance after an additional 24 weeks of follow-up.
With 55% of initial null responders receiving the drug for 44 weeks showing long-lasting viral clearance, the longer therapy appeared to be more effective, Kwo said.
He also noted that boceprevir for both durations boosted response rates well above what would normally be expected from standard therapy in patients without strong responses in the first four weeks.
He cited results from an earlier large trial in which less than 5% of early nonresponders to standard therapy eventually developed sustained responses.
Among patients showing strong responses in the first four weeks of interferon and ribavirin, sustained responses were seen in most.
More than 80% of those with initial reductions of three to four orders of magnitude in viral RNA levels had sustained responses, as did nearly 100% of those with reductions of at least four orders of magnitude or whose viral RNA became undetectable in the first four weeks.
Duration of boceprevir treatment appeared to make no difference in sustained virologic response rates in these patients.
But Kwo cautioned that the findings in these analyses involved relatively small numbers of patients. Only about 50 patients were considered null responders to the lead-in treatment, and similar numbers had relatively strong initial responses.
Overall, adding boceprevir after the four-week lead-in led to sustained responses in 56% of patients receiving boceprevir for 24 weeks, and in 75% of those taking the drug for 44 weeks, Kwo said. Both response rates were significantly (P<0.01)>
read more» Read more...
























 The irregular heartbeat known as atrial fibrillation is one of the toughest heart conditions to treat. Drugs aimed at restoring a normal beat are often ineffective and can have serious side effects. The anticoagulants that many people with A fib, as it’s known, need to take can react with other drugs and raise the risk of bleeding.
The irregular heartbeat known as atrial fibrillation is one of the toughest heart conditions to treat. Drugs aimed at restoring a normal beat are often ineffective and can have serious side effects. The anticoagulants that many people with A fib, as it’s known, need to take can react with other drugs and raise the risk of bleeding.





